" "quality sleep"
Anti-Snore Device
anti-snoring
Blue Light Blocking Glasses
Circadian Rhythm
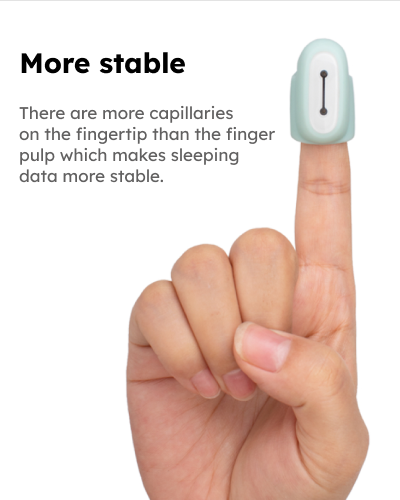
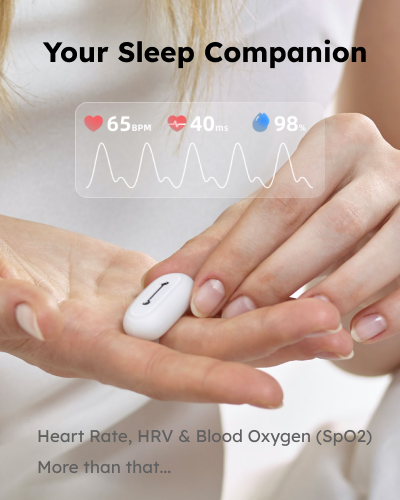
go2sleep
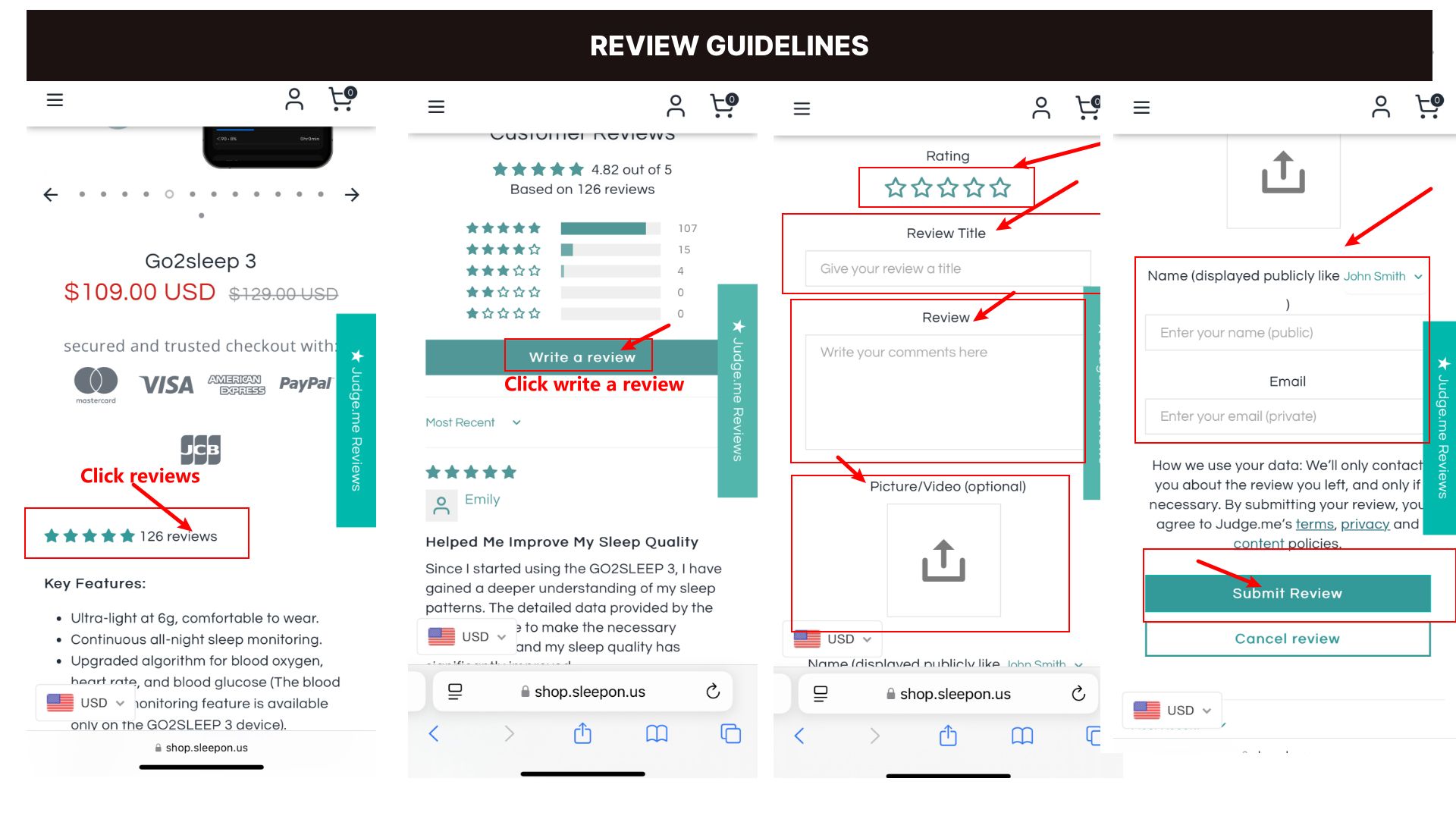
Go2sleep 3
Health
Health management
health technology
healthy living
healthy sleep habits
healthy sleep hours
healthy sleep hygiene
hrv
lack of sleep and mental health
less sleep will cause stress
loss of sleep
Obstructive sleep apnea
OSA
Oxygen Desaturation Index
Sleep
sleep and wellness
Sleep apnea
sleep cycle
Sleep disorders
Sleep Disturbances
sleep health
sleep hygiene
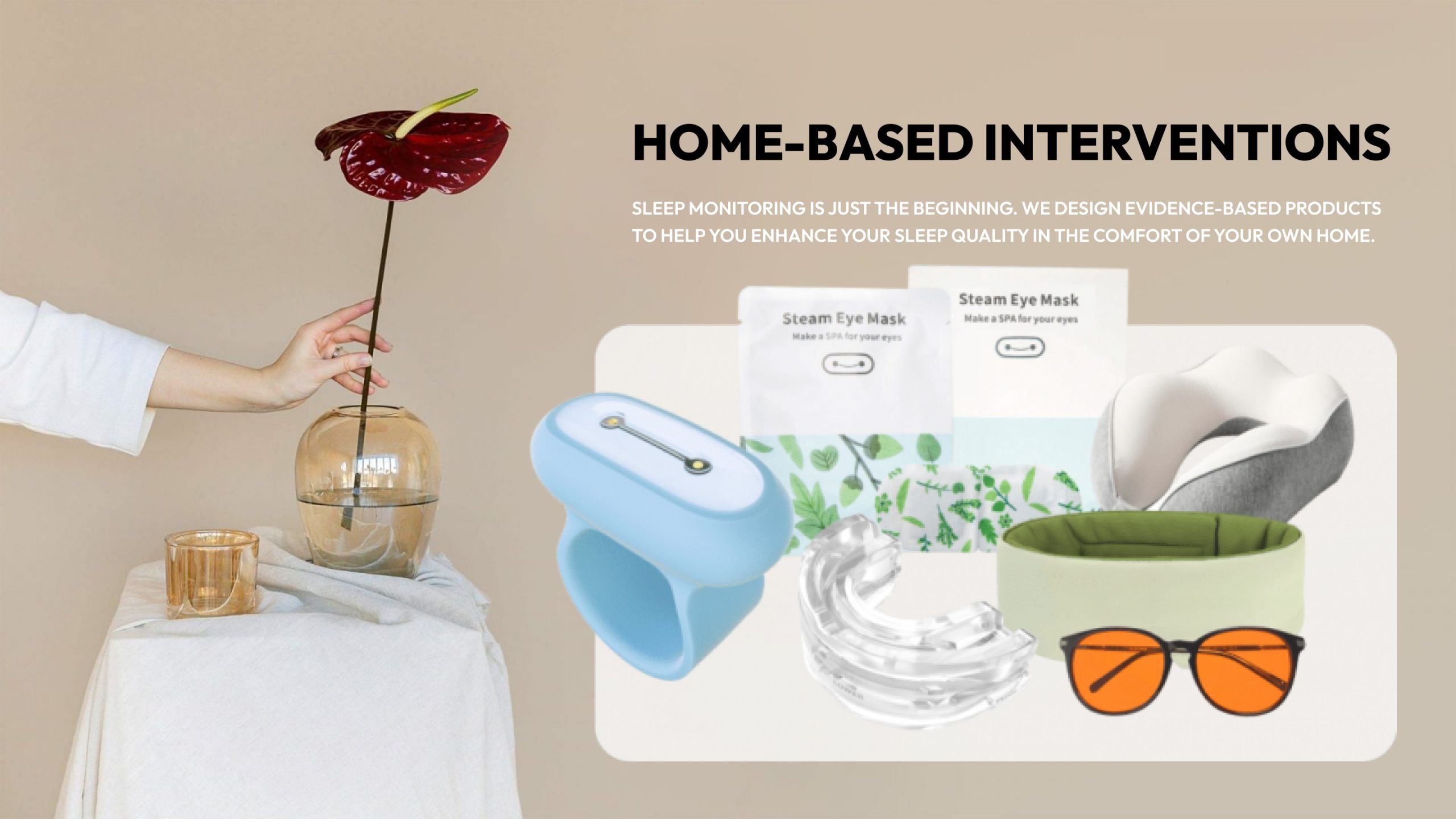
Sleep Improvement
sleep is the best medicine
Sleep monitoring
sleepon
Sleepon products
Sleep Patterns
Sleep Products
Sleep quality
sleep study test cost
Sleep Technology
sleep tips
sleep tracker ios
sleep tracking
snoring
special offer
Steam Eye Mask
Products
Company
Copyright © SLEEPON. All rights reserved.
SLEEPON keeps both Sleeponhealth and Sleepon.us due to the brand upgrading. We promise to provide the same products and service in both sites.